What Are The Limits On Cpt 96132
Always check with Medicare or other insurance providers regarding limits on the use of each CPT code for yourestrictions and regulations differ depending on your location.
There may be limits on the total number of hours that one provider can bill for in one day or one year for 96132 alongside other related codes for psychological and psychiatric services, although in some cases multiple services may be billed for the same date with the proper modifier code and documentation. The modifier code will depend on if the services were administered in the same encounter or the same date see below for more information on combining codes. Additional hours may be reimbursed with prior authorization, when medical necessity can be demonstrated, according to the APA.
Codes related to cognitive testing and evaluation often cannot be used for the same encounter when more general evaluation and management codes, such as 99308 or 99483, are also used .
Score An A For Coding Psychological And Neuropsychological Tests
CPT® codes for psychological and neuropsychological tests include tests performed by technicians and computers in addition to tests performed by physicians, clinical psychologists , independently practicing psychologists , and other qualified nonphysician practitioners . The payment amounts for tests performed by a technician or a computer are adjusted depending on whether the service was performed in a facility or non-facility setting.Psychological tests are generally used to assess an number of things, including behavior, personality, and IQ. Neuropsychological tests are used to assess brain activities such as learning and memory.
Test Interpretation And Feedback
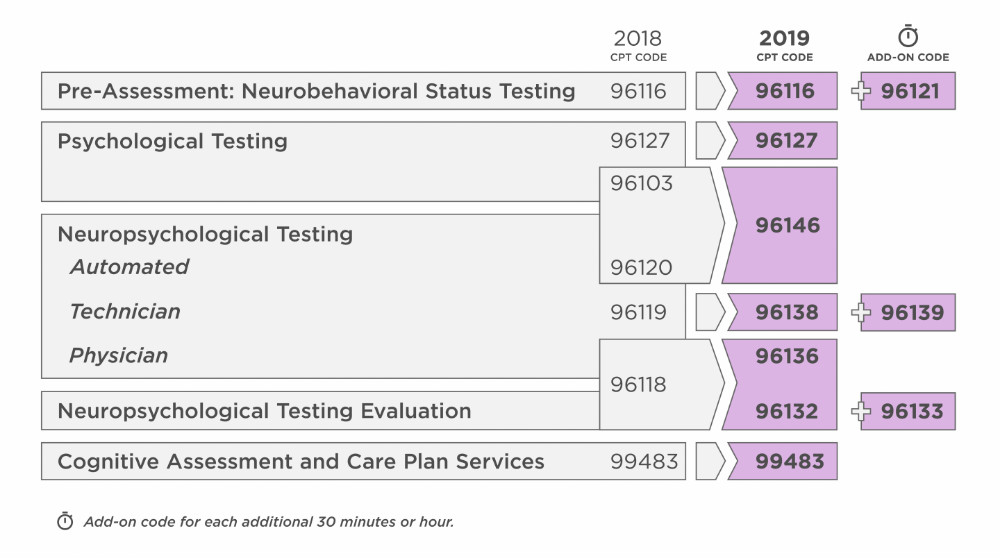
- Previously, BrainCheck advised using CPT code 96118 for the interpretation of results, when provided in a separate visit and integrated with results from other tests.
- Code 96118 will be eliminated and replaced with CPT code 96132.
- CPT 96132 is designated as Neuropsychological testing evaluation services by physician or other qualified healthcare professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report and interactive feedback to the patient, family member or caregiver, when performed first hour.
In part two, well cover the rationale behind these changes, what to expect with regards to reimbursement amount and what you need to do to prepare for the transition.
Also Check: Geometry Dash Theory Of Everything 2
Why Cpt Codes Are Essential For Clinicians
CPT codes are essential parts of practice management for clinicians and health care staff because they determine compensation and the practice’s overall success. To receive the correct reimbursement rates, clinicians must ensure the codes on insurance claim forms accurately reflect the services they provided before submitting the claims to insurance companies.
Phase : Psychological Testing
o Cognitive Testing: IQ and achievement testing to determine the strengths and weaknesses of a person’s thinking. General assessment, domains include: general awareness, attention, verbal comprehension, visual spatial ability, computation, abstract thought, impulsivity, problem solving, social comprehension, and judgment. Rule out gross learning disabilities.
o Emotional: Assess emotional functioning and assess for depression, anxiety, deficits in identity formation, obsessive/compulsive disorders, and sleep disorders. Assess personality functioning. Obtain data regarding developmental and emotional age. Obtain data regarding family dynamics.
o Behavioral: Evaluate substance abuse. Evaluate for trauma and abuse. Evaluate for risk of self-harm, aggression, and treatment compliance or flight. Detect malingering, deceit, and exaggeration. Screen for behaviors that are high risk, illegal, or violate the rights of others or major social values including substance abuse. Rule out thought disorders and screen for organic impairment.
o Executive Functioning: We believe EF skills should be evaluated in every client because EF Skills are highly correlated with outcome and EF skill development should be included into therapeutic treatment planning. Executive functioning assessment evaluates: self-regulation, problem solving, planning, organization, inhibition, meta-cognition , working memory, and accountability.
You May Like: How Do Noise Cancelling Headphones Work Physics
Psychological And Neuropsychological Testing Update Professional Claims Only
Blue Cross Blue Shield of North Dakota has reviewed guidance from the American Medical Association and the Centers for Medicare and Medicaid Services related to the allowable practitioners and Medically Unlikely Edit values for the Psychological and Neuropsychological Testing CPT codes.
The publication of the 2019 CPT Manual by the AMA added Other Qualified Healthcare Professional within the code description. To address this additional eligible provider, BCBSND updated the two codes below to allow psychologists to perform the following services:
- 96116 Neurobehavioral status examination by physician or other qualified health care professional, both face-to-face time with the patient and time interpreting test results and preparing the report first hour
- 96121 Neurobehavioral status examination by physician or other qualified health care professional, both face-to-face time with the patient and time interpreting test results and preparing the report each additional hour
BCBSND reviewed clinical documentation and standards of practice for these services. The findings supported the change in the MUE values associated with the two CPT codes below. The MUEs for 96137 and 96139 were increased from 11 units to 17 units with an effective date of January 1, 2019.
Due to the above MUE changes, BCBSND has revised the Correct Coding Guidelines and MUE Revisions Addendum available at .
New Cpt Codes For Behavioral Health Services
Every year, health professionals can expect revised or new mental health CPT codes. According to the American Psychological Association, as of Jan. 1, 2020, psychologists must use new therapy CPT codes to get reimbursed for health behavior assessment and intervention services from third-party payers. Providers use these services to address psychological, emotional, cognitive, or behavioral issues that impact the treatment of a physical health problem. Psychologists may provide these services to an individual, group, or a patient’s family to help the client cope with physical health conditions.
HBAI codes require a physical health diagnosis or an ICD code and are not for mental health services. Here are the code revisions.
For additional information about the 2021 E/M coding changes, check out our blog post here.
Read Also: Kendall Hunt Geometry Answer Key
Cpt Codes For Psychological And Neuropsychological Testing
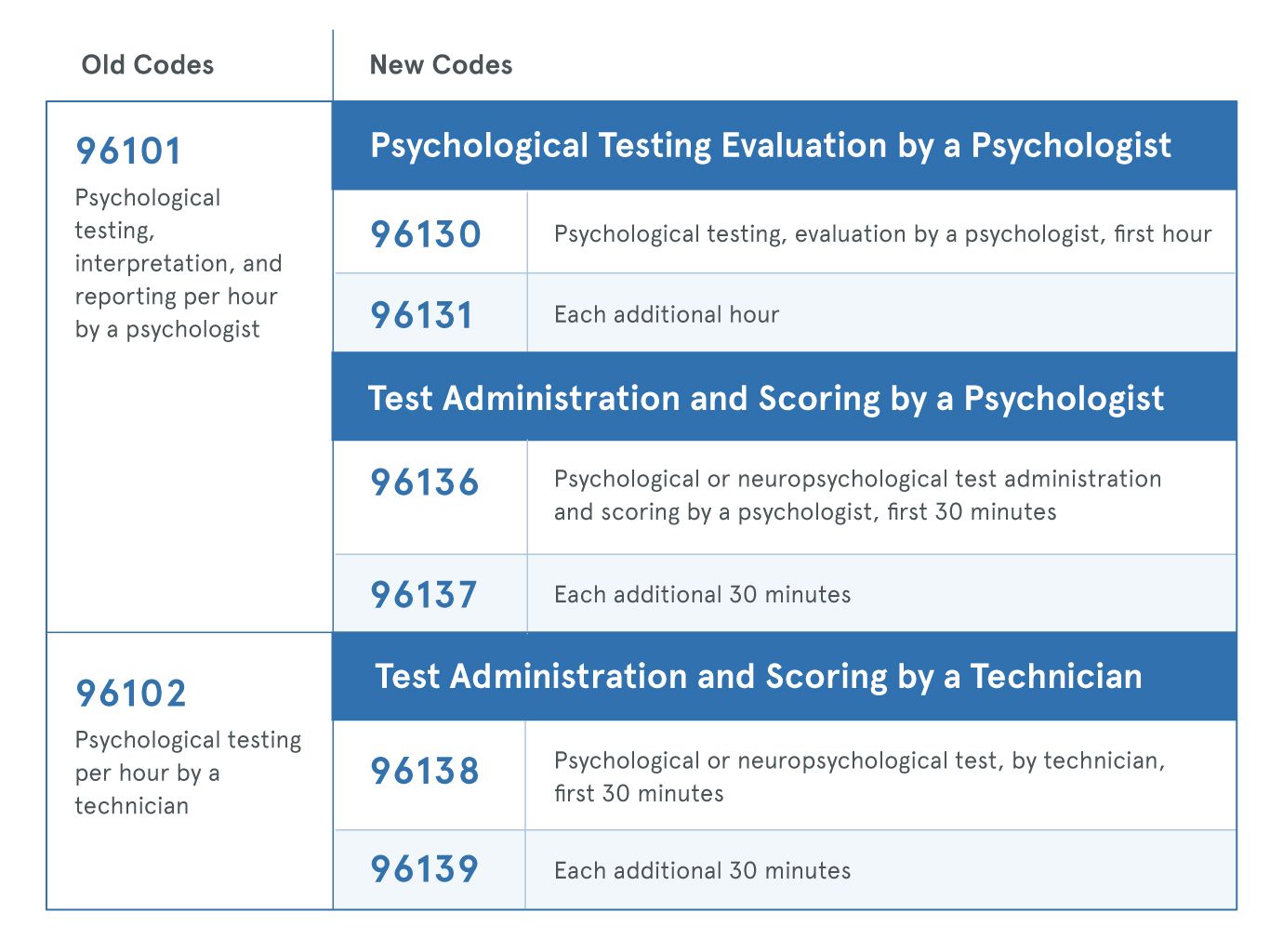
The American Medical Association issued extensive changes to CPT codes used for psychological and neuropsychological testing for dates of service on and after Jan. 1, 2019. This impacts both payers and providers. The AMA modernized the coding structure to separate evaluation services from testing and administration services only. The changes will more accurately describe the work performed when multiple hours of technical and professional are required. Coding changes will impact psychiatrists and psychologists who perform psychological and neuropsychological testing services. Implementations of the new CPT codes are mandatory non-compliance is a HIPAA violation. Here are the coding changes psychologists should be aware of:
E2E Medical Billing Services is assisting mental health/behavioral health providers for more than 5 years and has expertise in implanting these updates to increase practice reimbursement. Need more guidance on the new CPT codes? You can call us at or write to us at
What Is The Role Of Cbs Health In Billing For Cpt Code 96132
Many healthcare providers bill for administering a CBS Health protocol to a patient as a neuropsychological assessment, providing income for the practice and ensuring that any investment in CBS Health has a positive return.
Aside from direct reimbursement for an assessment, CBS Health can play a key role in making billing easy, such as:
- Providing a report that documents the results of an assessment, as well as metadata such as the time an assessment was administered, for easy documentation in an EHR or future reference.
- Generating easy-to-read reports that aid in interpretation of standardized results, interactive feedback with the patient, clinical decision making, and treatment planning, all of which fall under the time billed for CPT code 96132.
- Complementing other assessment results in order to aid in diagnosis, thereby proving medical necessity for other services that may be billed during the same session or at a later date.
- Combining mental health assessments for depression, anxiety, and ADHD in the same platform as cognitive assessments, so that mental health questionnaires can justify the need for cognitive testing, and vice versa, with a single email to a patient.
Whether you are already using our platform, or are considering adding reimbursable cognitive assessments to your practice, get in touch with us any time to discuss how to best make use of CBS Health.
You May Like: How To Pass Ap Human Geography
The Most Common Cpt Codes Used By Therapist
There are over 8,000 CPT codes out there, however, the good news is only 24 of these codes are designated for psychotherapy. The even better news is that you, as a therapist, will likely only use about 8 of these regularly. The most common CPT codes used by the therapist are:
| CPT | |
| 90839 | Psychotherapy for a crisis, 60 minutes . |
As mentioned before, there are over 8,000 CPT codes out there, however, the good news is only 24 of these codes are designated for psychotherapy. The even better news is that you, as a therapist, will likely only use about 8 of these regularly. Still choosing the best-suited CPT code for the therapy could be a tricky task.
E2E Medical Billing Services having more than 5 years of experience in medical billing for psychiatric and psychological services. Using the exact CPT code will ensure no denials, prompt payment, and ultimately smoother cash flow for your practice. To know more about our mental health/ behavioral health billing services, you can call us at or write to us at
Psychological And Neuropsychological Tests
CMS released questions and answers on psychological and neuropsychological tests that are billed under the CPT code range 96101-96125. These Frequently Asked Questions provide clarification on Medicare billing and payment policy for these testing codes when performed by technicians, computers, physicians, clinical psychologists, independently practicing psychologists and other eligible qualified nonphysician practitioners. The scenarios under the FAQs also address situations where more than one of these testing codes can be billed for services furnished to the same patient.
Don’t Miss: What Does Commensalism Mean In Biology
Distilled Guide To Mental Health Cpt Codes
If you are just starting out or just beginning to deal with managed care, keep it simple.
CPT Codes appear far more complex from the outside looking in. Make a quick cheatsheet.
Dont worry about memorizing all the CPT Codes or even all of the mental health ones. You will likely just use just a few individual codes.
Memorize the relevant codes and use google or other references to find the correct CPT codes for more unique scenarios.
And if all of that sounds like too much trouble, offload the work to us. You wont have to know one CPT code from another to get your billing paid in full.
Typical Reimbursements By Type Of Therapist
| Type of Therapist |
| ~$70-80 |
These rates can vary significantly therapist to therapist but are good benchmarks for comparison.
How about CPT Codes? How do they affect the rate of reimbursement? This is a difficult and complex calculation, depending on the level of education, location, and license. The AMA has created a code search feature on their website that shows payment based off CPT Code and location.
This information is somewhat incomplete and is based off medicare payments and does not specify a number of other important factors. However, this tool is still very useful to compare the relative value CPT Codes against one another.
Private insurance will be correlated with some deviation from these numbers.
Don’t Miss: Algebra 1 Eoc 2015
Supervision Requirements Depend On Provider
All diagnostic tests are assigned a certain level of supervision. Generally, diagnostic tests require a physician to provide the appropriate level of supervision for such tests. That is, the physician must either provide general, direct, or personal supervision. However, for diagnostic psychological and neuropsychological tests , there is a regulatory exception ) that allows either a CP or a physician to provide the required general supervision for diagnostic psychological and neuropsychological tests. NPPs, such as nurse practitioners and clinical nurse specialists , and physician assistants , who personally perform diagnostic psychological and neuropsychological tests are excluded from the supervision requirements for diagnostic tests. However, they must meet the collaboration and physician supervision practice requirements under their respective benefits.
Cpt Codes Covered If Selection Criteria Are Met:
96116 Neurobehavioral status exam , per hour of the psychologist’s or physician’s time, both face-to-face time with the patient and time interpreting test results and preparing the report 96121 Neurobehavioral status examination , by physician or other qualified health care professional, both face-to-face time with the patient and time interpreting test results and preparing the report each additional hour 96125 Standardized cognitive performance testing per hour of a qualified health care professional’s time, both face-to-face time administering tests to the patient and time interpreting these test results and preparing the report 96130 – 96131 Psychological testing evaluation services by physician or other qualified health care professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report, and interactive feedback to the patient, family member or caregiver, when performed 96132 – 96133 Neuropsychological testing evaluation services by physician or other qualified health care professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report, and interactive feedback to the patient, family member or caregiver, when performed 96138 – 96139
Don’t Miss: Prince Jackson Biological Father
Psychiatry Evaluation And Management Codes
Psychiatrists may use E/M codes to bill for evaluation and management services either alone or with psychotherapy. For psychiatrists and other physicians, psychotherapy is an add-on code to the primary E/M service.
Cpt Coding For Therapy
CPT coding for psychotherapy doesnt have to be difficult! There are an overwhelming amount of total CPT Codes , however only 24 are specifically designated for psychotherapy and other mental health services.
To make matters even simpler, nearly all therapists will regularly use an even smaller subset of these 24.
CPT is a large and dynamic code set that changes year to year, but the psychotherapy codes seldom change.
The most recent change for psychotherapy codes took place in 2019, then 2013, and previously 1998.
To ensure your coding is current and up to date, consider using a billing service instead of having to remember all the codes.
Also Check: Who Is Generally Recognized As The Founder Of American Psychology
Usage Patterns Of Recovery Record For Clinicians That Should Qualify
Always check with the payer for coverage of these billing codes, rates and any extra requirements. Use Recovery Record for Clinician’s built-in outcomes collection tool to collect a set of relivant assessments digitally from the patient. This can be done in session or between sessions. Recovery Record will automatically score them for you. Use the scores to help inform the care plan and areas of focus. Provide feedback to the patient either during the next session or with a quick face-to-face call through Recovery Records’s video call feature. Export or screenshot the assessments responses and scores and add to the patient’s medical record.
You can choose two or more of Recovery Record’s builtin assessments as part of the Outcomes Tool. Recovery Record will collect the repsonses and score them for you.
- EPSI
- GAD-7
Phase : Interview And Information Gathering
At the start of the assessment, all of the important stake holders are identified. These typically include client, parents, significant other, therapist, referral consultant, psychiatrist, and other professionals or programs that may have insight. Parents and Client are given a Parent Questionnaire to fill out prior to their interview to create an outline of relevant historical information which is then detailed during the interview. Parents can submit their own narrative or timeline which can help tremendously. Calls are scheduled with prior treatment providers. The purpose of the interviews is to gather information, as well as understand the perspective and opinions of the interviewee.
Also Check: Who Are Paris Jackson’s Biological Parents
American Hospital Association Disclaimer
The American Hospital Association has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
How To Use The Correct Cpt Code In Psychiatry
The CPT code set is a complex system. It is not always easy to determine if you’ve met the required elements to code appropriately for the maximum reimbursement amount. It may help to break the process down into steps for new and established patients.
First, you might bill two types of psychiatric service or procedure codes for new patients. These are:
- E/M codes
- Psychiatric diagnostic evaluation codes
Depending on the situation and time involved, it may be appropriate to bill for both codes. Here are a few guidelines to follow.
- E/M: Use E/M codes when evaluating a new medical issue. With the AMA’s 2021 coding changes, you can select an E/M code based on the complexity of medical decision-making or the total time you spent on the patient’s care on the day of the encounter. If you provide E/M services with a psychotherapy add-on code, you must choose a code based on medical decision-making and not total time.
- Psychiatric diagnostic evaluation: Use psychiatric diagnostic evaluation codes for a diagnostic assessment. You may need to use these codes more than once if it takes more time to complete the initial evaluation.
Regarding established patients, the rules allow you to bill an E/M service with every psychotherapy visit, but they don’t require you to do so with every encounter. Only bill E/M services if you addressed and documented a separate medical issue during the visit.
You May Like: Exponent Rules Worksheet 8th Grade